Quality shapes the reality of every healthcare encounter. When a person steps into a healthcare organisation, they bring trust, fear, and expectations that their well-being will be protected. The stakes are high because healthcare affects lives in ways few other industries do. This makes quality assurance (QA) in healthcare a central pillar of modern healthcare delivery. Reliable systems help prevent errors, strengthen patient safety, and create a care environment people can trust.
Global data makes the urgency clear. Patient harm slows worldwide economic growth by approximately 0.7% each year and contributes trillions of dollars in indirect financial loss. Safety initiatives significantly reduce preventable harm, and patient engagement alone can lower harm by up to 15%. These figures demonstrate why quality assurance is crucial: it enhances patient outcomes, reduces medical errors, and contributes to cost savings at a time when healthcare costs continue to rise.
This article will introduce you to QA in healthcare, explain how quality assurance differs (quite a bit) in healthcare compared to other sectors, and explore how standards, frameworks, and modern tools contribute to a safer, clearer, and more patient-centred care.
What Is Quality Assurance in Healthcare?
Quality assurance in healthcare is a structured, preventive system designed to maintain consistent, high-quality care across all stages of healthcare delivery. It focuses on preventing errors, aligning teams with evidence-based practices, improving patient safety, and supporting patient satisfaction scores. QA in healthcare enhances communication, documentation, and clinical procedures, ensuring patient care remains predictable, safe, and compliant with regulatory requirements.
Healthcare settings heavily rely on processes that leave little room for variation. Quality assurance helps keep things organised, enabling you to meet regulatory requirements and adopt effective QA systems that support long-term reliability. Strong QA frameworks also help reduce the risk of adverse events and support patient outcomes, especially in environments where complex treatments, new technologies, and time-sensitive decisions intersect.
Healthcare differs from other industries because lives and long-term well-being quite literally depend on every process. This makes quality assurance here inherently different. The work must address clinical complexity, emotional needs, and ethical responsibilities that influence patient expectations and shape the overall experience.
QA vs QC vs QI
QA in healthcare, quality control (QC), and quality improvement (QI) work together to protect patients across their journey. Each plays a distinct role, and understanding how they connect strengthens the entire system by creating consistency, reducing risk, and supporting safer care delivery across all clinical settings.
Quality assurance creates preventive structures. It focuses on designing procedures, communication pathways, staff training, and documentation routines that prevent errors and ensure quality. QA establishes a foundation that guides daily practice and reduces risk before it occurs.
Quality control identifies defects through inspection. It evaluates whether processes meet the required quality standards. QC plays a strong role in laboratories, pharmacy workflows, and digital patient-facing systems that demand precision.
Quality improvement supports long-term development. It uses continuous monitoring and outcome data to refine healthcare delivery. QI helps organizations stay responsive and adaptable by learning from performance trends.
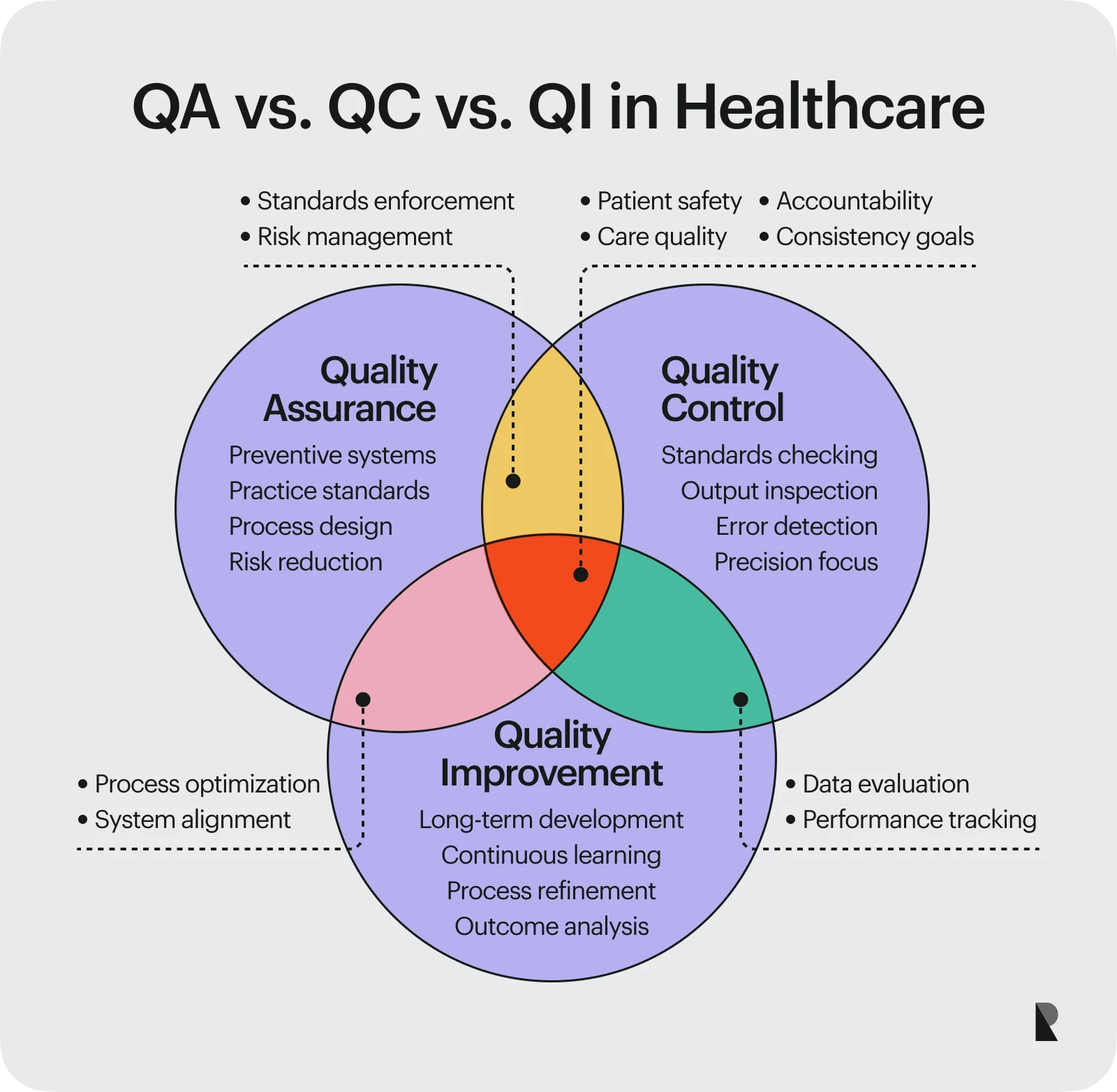
When QA, QC, and QI work together, they help prevent errors, detect issues early, and drive improvements that keep healthcare delivery safe, consistent, and aligned with patient needs. This collaboration also strengthens accountability, supports staff training, and reinforces long-term clinical reliability across departments.
Core Principles of Healthcare Quality Assurance
Quality assurance in healthcare is grounded in ethics, evidence, and accountability. These principles enable organizations to support patient safety and deliver genuine value to the communities they serve by fostering trust and delivering consistent care. The following sections describe the core components that guide effective QA work and strengthen both clinical and operational performance.

1. Patient-centered and ethical care
Patient-centered care defines quality assurance in healthcare. It emphasizes safety, dignity, and trust by focusing on the patient experience, preventing errors, and responding clearly to patient expectations. Ethical oversight helps protect against harm and supports transparency in clinical decision-making. Feedback loops enable organizations to learn directly from the individuals receiving care, thereby strengthening patient outcomes and enhancing the overall experience.
2. Evidence-based standards and clinical guidelines
Evidence-based care creates a reliable foundation for quality assurance. Healthcare organizations adhere to clinical research, validated protocols, and established guidelines that represent the gold standard in modern medicine.
Many institutions rely on a committee for quality or national committee bodies that review new data and update clinical practices. These guidelines help teams establish consistent and effective QA processes that reduce risk and enhance healthcare delivery.
3. Continuous monitoring and data-driven improvement
Continuous monitoring plays an essential role in healthcare QA. By tracking performance metrics, patient outcomes, and workflow patterns, healthcare teams understand where risks develop and how to prevent errors more effectively.
Real-time dashboards and analytics highlight where improvement opportunities exist. These data-driven insights contribute to cost savings by helping reduce waste, streamlining processes, and identifying preventive measures at the earliest stage.
4. Accountability, transparency, and professional responsibility
Quality assurance depends on a culture of responsibility. Transparent reporting, internal audits, and reliable documentation help teams meet regulatory requirements and maintain high-quality standards.
When healthcare professionals feel confident in reporting concerns and participating in improvement activities, organizations gain a better understanding of their systems and improve patient safety across all departments. This approach enhances the patient experience and contributes to improved long-term patient outcomes.
Key Quality Standards and Accreditation Frameworks
Quality assurance systems depend on recognised standards that guide healthcare organisations in delivering consistent, safe, and effective care. These frameworks provide structure, credibility, and a clear path for meeting regulatory requirements while ensuring patient outcomes are protected. The following frameworks shape the way hospitals, clinics, and healthcare-facing systems operate today.
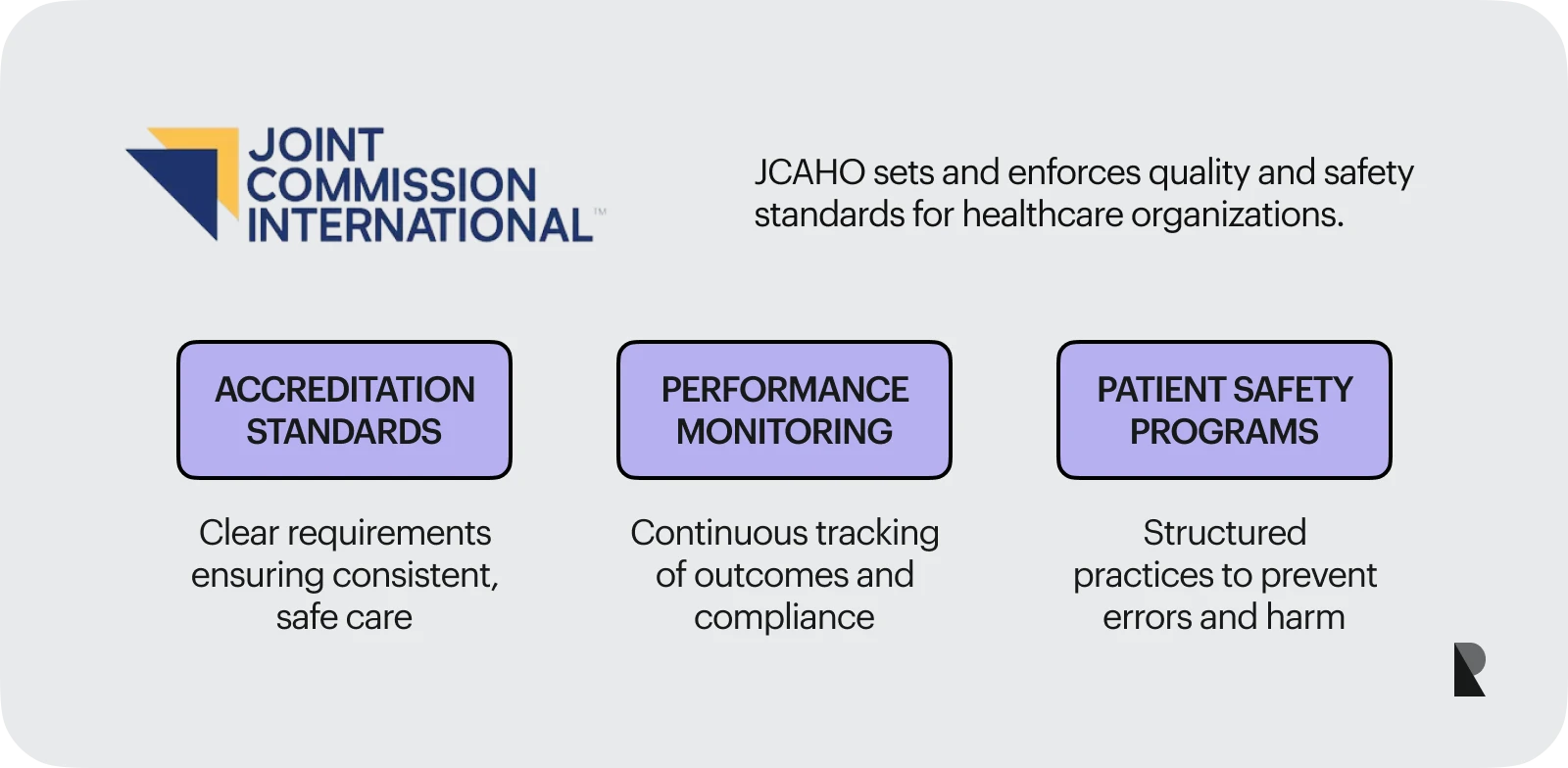
The Joint commission (JCAHO)
The Joint Commission plays a leading role in shaping quality assurance in the United States. JCAHO accreditation evaluates patient safety, performance, and compliance with quality standards. Organisations with JCAHO accreditation benefit from structured guidelines, reduced medical errors, and stronger patient satisfaction scores. These expectations help stimulate a culture where continuous monitoring and improvement are integral to daily operations.
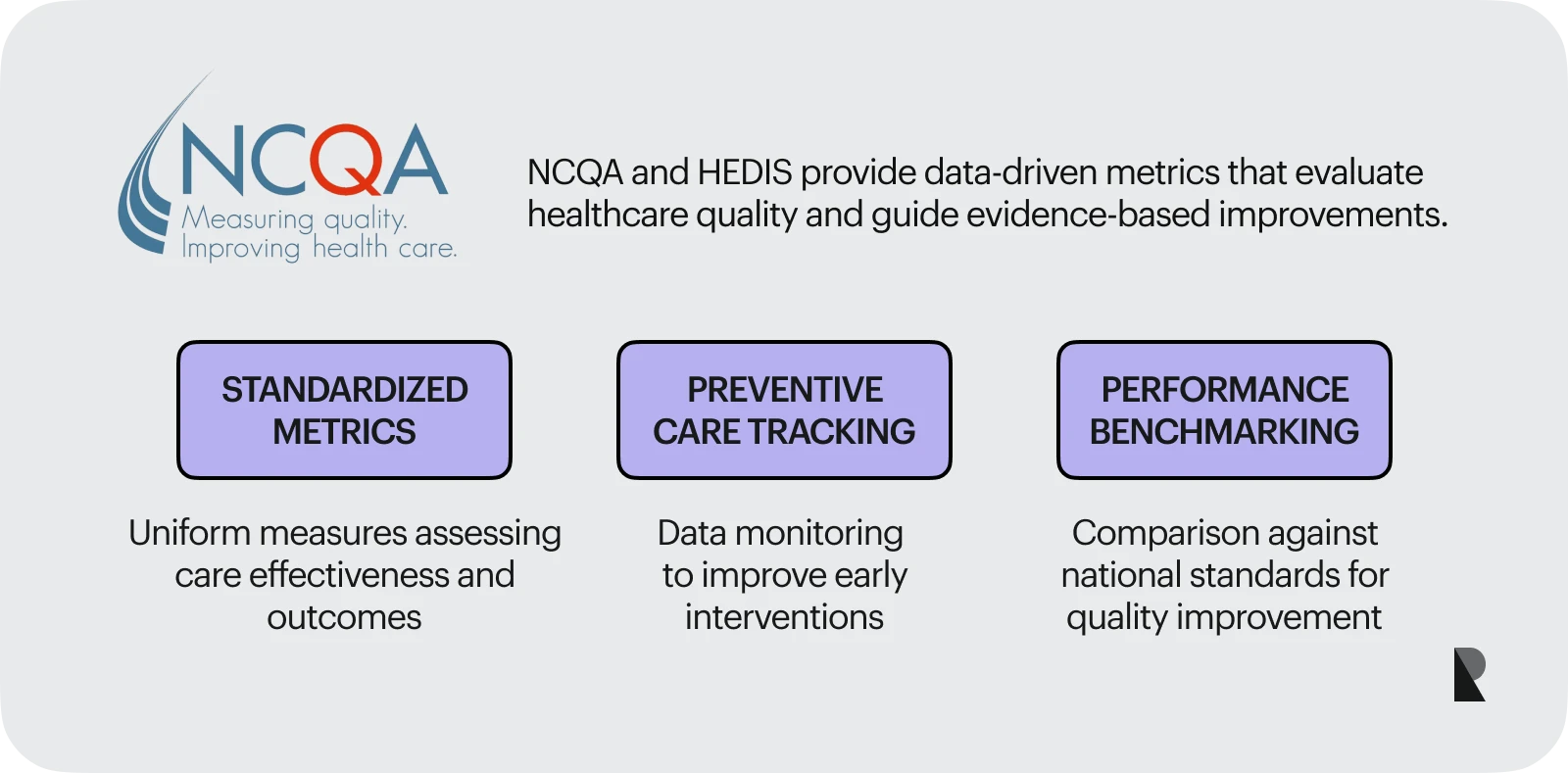
NCQA and HEDIS quality measures
The national committee for quality assurance sets data-driven standards for evaluating health plans and providers. HEDIS measures track preventive care, treatment outcomes, and service effectiveness. These metrics enable organisations to assess their performance, strengthen patient-centred practices, and align with evidence-based benchmarks that enhance healthcare delivery.
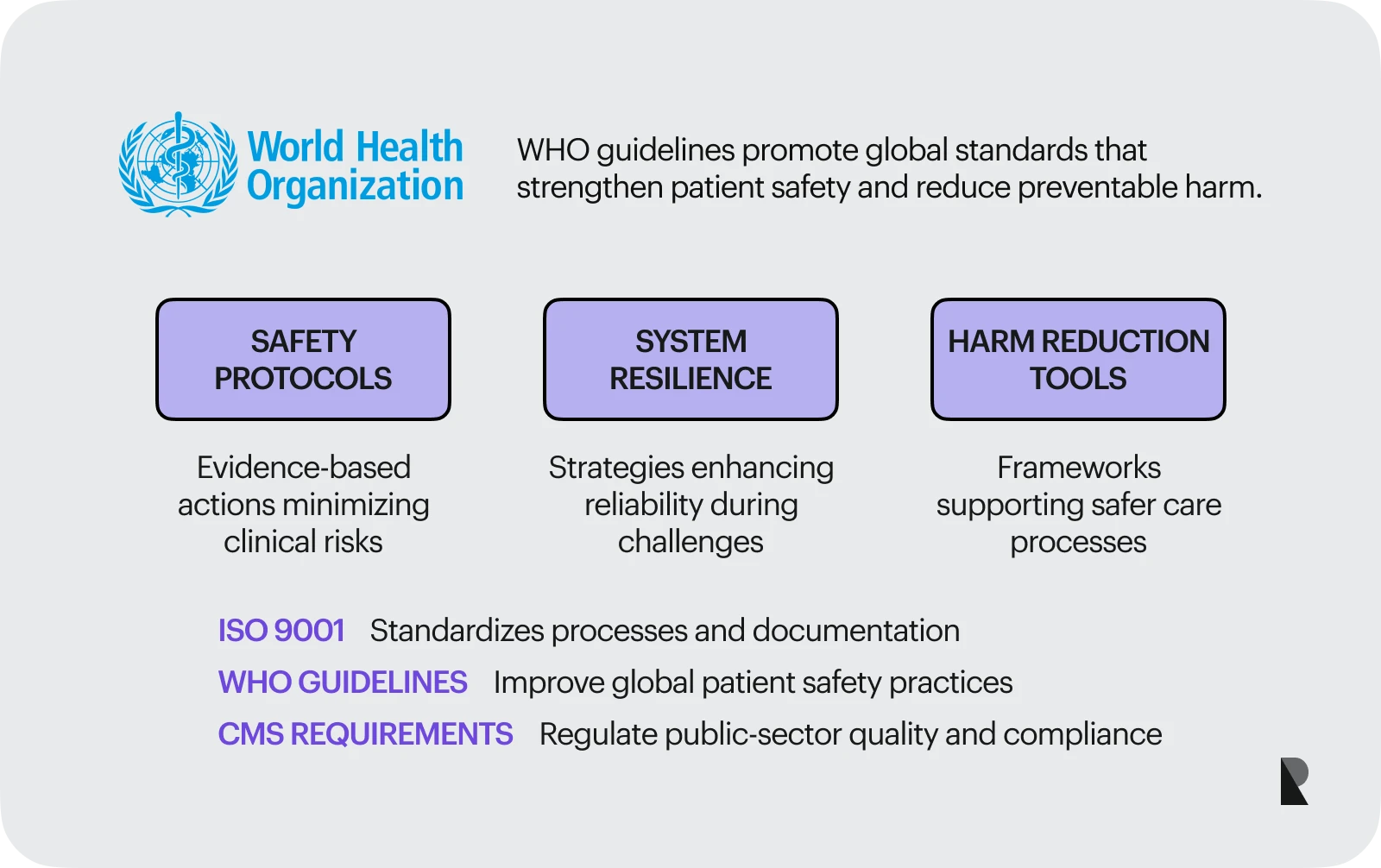
Other QA frameworks (ISO, WHO, CMS)
ISO 9001 supports strong documentation and consistent process management. WHO guidelines focus on patient safety practices that reduce preventable harm and improve system resilience.
CMS requirements help regulate public-sector quality standards, patient safety priorities, and compliance expectations. Together, these frameworks support effective qa in healthcare and help organisations stay accountable in a constantly evolving environment.
QA Tools and Technologies in Healthcare
Technology has become one of the strongest supports for QA in healthcare. As healthcare delivery spans multiple departments, digital platforms help teams stay aligned, reduce variation, and maintain quality standards in rapidly evolving environments. These systems handle documentation, track performance, support staff training, and guide clinical decisions with reliable information. They reduce room for error in processes where accuracy directly influences patient outcomes.
Technology also changes how healthcare organisations respond to complexity. With more patient-facing systems, more data, and more interdependent workflows, quality assurance depends on tools that bring clarity to operations.
Digital platforms enable organisations to stay current with regulatory requirements and establish a predictable structure for tasks that previously relied on manual oversight.
Core capabilities of QA software
Modern QA software connects large amounts of information into a single system that teams can use throughout the QA cycle. Dashboards visualise performance trends, alerts highlight potential issues, and documentation tools support consistent communication. With this structure, healthcare organisations gain a clearer understanding of how decisions, handoffs, and workflows influence patient outcomes.
These capabilities support cost savings by eliminating unnecessary steps, identifying inefficiencies, and enhancing accuracy across patient care processes. When data is organised and accessible, teams can identify patterns more quickly and take action before issues escalate.
Strong QA software also supports staff training by providing standardised reference points and real-time information on performance trends. These strengths enable organisations to remain consistent even during periods of high demand or rapid change.
Compliance, security, and data integrity testing
Every healthcare organisation must protect sensitive information and uphold regulatory requirements. This makes security testing a key part of quality assurance. Healthcare systems handle a significant amount of sensitive data, and any vulnerability compromises the safety, trust, and continuity of care. Testing focuses on system reliability, data integrity, and the confidentiality of patient records.
HIPAA, GDPR, and similar frameworks expect organisations to maintain strong safeguards. As healthcare delivery increasingly relies on digital records and interconnected systems, the importance of high-quality testing continues to grow.
Healthcare QA incorporates these processes into routine operations to ensure that systems remain reliable and information remains protected. These practices reduce the risk of medical errors caused by missing data, incorrect entries, or disruptions to digital systems.
Usability testing for patient-facing systems
Digital care is now part of everyday healthcare delivery. Patients schedule appointments online, access test results through secure portals, and communicate with their providers through mobile apps. These interactions influence how patients experience care, so quality assurance must evaluate how well these systems support real needs.
Usability testing identifies where digital tools cause confusion or slow the patient journey. It evaluates clarity, accessibility, readability, and navigation. Observing real behaviour offers direct insight into how people interact with their healthcare organisation, which helps teams refine design and improve patient outcomes. Better usability reduces misunderstandings, supports patient expectations, and contributes to more consistent patient-centred care.
Case Study: Implementing QA in a Healthcare Organization
A regional hospital experiencing an increase in medical errors and declining patient experience ratings decided to establish a stronger quality assurance framework. They faced growing patient complexity, expanding digital systems, and inconsistent handoffs between teams.
Leaders saw the need for a unified approach that aligned evidence-based guidelines, technology, and professional responsibility. The hospital initiated the process by forming a quality committee to review existing processes and identify areas for improvement. They compared documentation practices, communication patterns, and clinical pathways with national committee recommendations. This comparison revealed variation that affected patient outcomes, especially during critical transitions of care.
The team introduced a structured QA cycle that included routine audits, continuous monitoring, and clear performance expectations. Technology played an important role. New QA software centralised documentation, automated alerts, and created real-time dashboards that showed where workflows were drifting away from quality standards. This visibility enabled teams to respond quickly to emerging issues, rather than waiting for quarterly reviews.
Patient-centred improvements followed. Staff training focused on clearer communication, consistent documentation, and respectful patient interactions. The hospital also refined its patient-facing systems. Usability testing highlighted where patients struggled with digital tools, which led to revised layouts, simpler instructions, and updated forms. These adjustments supported smoother interactions and reduced confusion during follow-up care.
Within a year, medical errors decreased, patient satisfaction scores improved, and clinical teams reported clearer expectations across departments. These types of results align with broader industry findings that demonstrate how structured quality systems contribute to improved patient outcomes. Recent national analyses found that hospital performance in early 2024 exceeded pre-pandemic levels, with more than 20% higher-than-expected survival rates and an estimated 200,000 patients avoiding fatal outcomes thanks to improved safety practices.
Conclusion
Quality assurance in healthcare builds safer systems, supports patient-centred care, and reduces the likelihood of medical errors. It brings together preventive frameworks, evidence-based guidelines, continuous monitoring, and clear accountability, enabling teams to deliver high-quality care with consistency. These practices also contribute to cost savings by removing inefficiencies and reducing preventable harm.
As healthcare becomes more digital, organisations increasingly collaborate with software development companies to upgrade patient-facing platforms, improve qa software, and modernise data systems. These partnerships support long-term quality goals and help organisations stay aligned with regulatory requirements.
Quality assurance will continue to evolve as new standards, tools, and research emerge. Organisations that invest in strong frameworks, clear communication, and reliable data practices build trust, improve patient outcomes, and create a healthcare experience grounded in safety and high-quality care.
Dec 4, 2025
